Healthcare has progressed a lot, but there's still a ton we don't understand about our bodies. Check out these five incredible medical mysteries that scientists can't figure out.
Our knowledge about the human body is growing faster than ever. Back in 1950, it took around 50 years for new medical information to double—nowadays, it happens every 73 days. Yet, there's still so much we haven't figured out about human biology. Scientists believe there are approximately 4,000 types of bacteria in our gut, but we're in the dark about what 70% of them actually do. The reasons behind dreaming, diverse blood types, and unique fingerprints are still unclear. Just this year, researchers found a new body part related to chewing our food.
Despite our modern scientific progress, doctors still find themselves puzzled by certain medical mysteries. Thankfully, with our rapidly expanding knowledge, they're also solving cases that were once perplexing. However, five particular medical marvels continue to baffle us, defying explanation.
The Chapel That Beat Cancer
Sitting at the church one evening, pouring out his heart to God, Greg envisioned making a meaningful contribution before leaving this earth. His commitment involved restoring the church's peeling paint, leaking roof, damaged steps, and decaying floorboards. Greg approached the church's association with a proposition: complete renovation in exchange for a key to the front door for personal worship. Despite a slow recovery from three rounds of chemotherapy, 40 radiation sessions, and a weight loss of 66 pounds, they agreed.
Remarkably, as Greg worked on the church's rehabilitation, his strength increased daily. He even dispensed with the potent prescription pain medications prescribed by his oncologist. Medical scans delivered surprising results – his tumors were shrinking. Four years and 23 days post-diagnosis, Greg's doctors removed his feeding tube, initially deemed a lifelong necessity. Today, Greg is officially in remission, free from follow-up tests.
The church, after five years of Greg's dedicated efforts, has regained its former glory. Greg anticipates continued involvement in its maintenance, expressing a belief that, "While I was restoring the church, God was restoring me."
The Role of a Lifetime
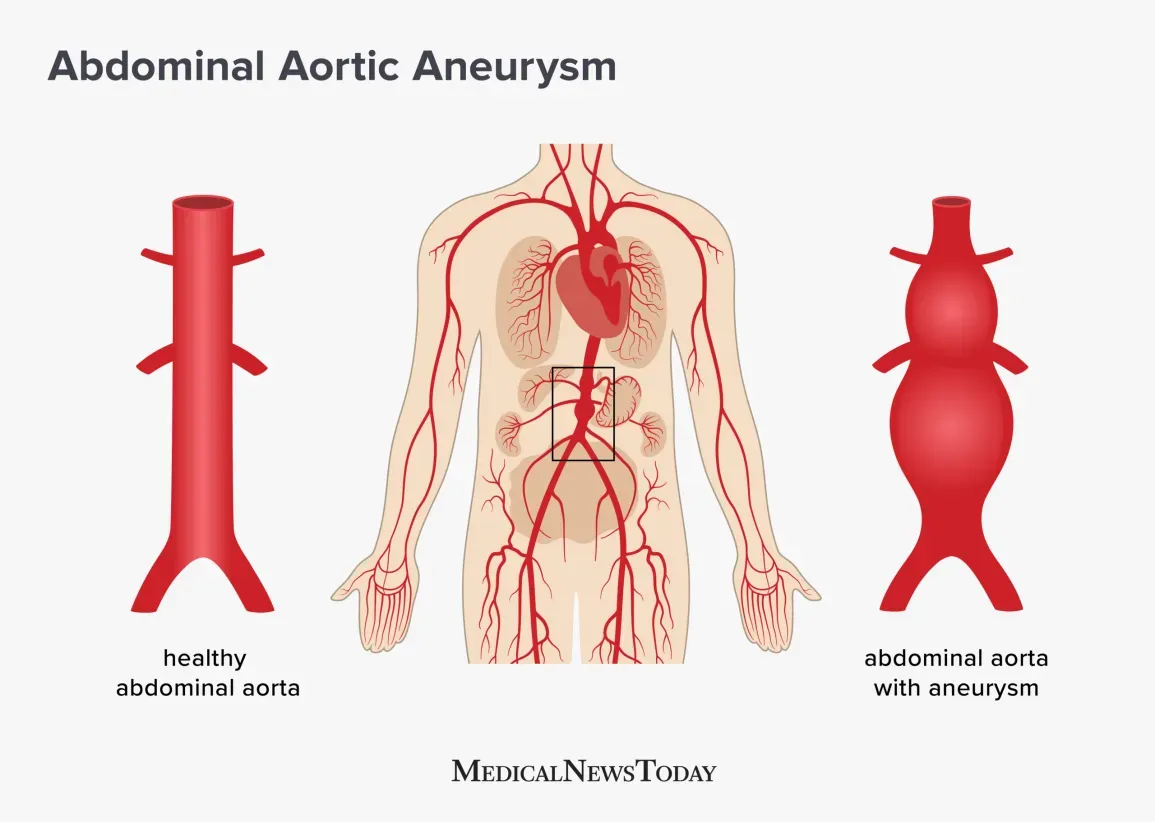
In an unexpected role reversal, Jim Malloy found himself embodying this silent killer as a "medical actor" one day in February 2013. A 75-year-old retired engineer, Jim had taken on various simulated medical issues over the years to help University of Virginia School of Medicine students practice their diagnostic skills. It was merely a lighthearted part-time retirement gig.
During one session, when third-year medical student Ryan Jones entered the room, Jim adhered to his AAA script, complaining of lightheadedness and stomach pain. However, when Ryan pressed on Jim's abdomen, he was astonished to feel a pulsing mass – an apparent genuine aneurysm.
"I stepped quickly back, confused," recalls Ryan. "I tried to get Mr. Malloy to break character and tell me that he knew he had an aneurysm. But he wouldn't."
Jim's attending physician advised him to consult a cardiologist, though Jim found it challenging to take the advice seriously. He believed he had no symptoms, having received a clean bill of health from his primary care doctor just two weeks earlier.
An ultrasound revealed Jim's AAA measured six centimeters, with the potential for rupture. Urgent surgery was scheduled, and a stent was inserted to deflate the aneurysm, ultimately saving his life. Jim, oblivious to the situation, acknowledges, "I had no idea anything was going on, and I would have just gone about my business. I'd probably be dead."
Ryan concurs, emphasizing the extraordinary coincidence of Jim volunteering for that specific case. If Jim had been simulating a different condition, the crucial examination might not have taken place. Jim was undeniably in the right place at the right time.
No one appreciates this life-saving stroke of luck more than Jim's wife, Louise. Post-surgery, she encountered two women whose husbands succumbed to AAA-related complications. Their gratitude towards Ryan is immeasurable.
Fighting a Lethal Amoeba That Devours the Brain
There was no other way to put it. It seemed unimaginable that just the day before, Kali and her friends had been joyfully playing king of the hill at a water park near Benton, Arkansas, before her severe headache and persistent nausea began. The heartbreaking news from doctors informed her parents that Kali likely contracted a brain-eating amoeba when water entered her nose. This microscopic organism traveled through her olfactory nerve into her brain, initiating the devouring of brain tissue, a condition known as primary amoebic meningoencephalitis. The medical prognosis was grim, with a 99 percent fatality rate—only two individuals in North America had survived this rare infection. "We had to tell her parents that it was very likely she would not be alive in 48 hours," revealed Dr. Matt Linam, the infectious disease specialist overseeing her treatment.
Arkansas Children’s Hospital immediately sprang into action. They administered antifungals, antibiotics, and an unconventional German drug obtained from the CDC. Kali's body temperature was lowered to 93 degrees, inducing a medically-induced coma to mitigate brain swelling. She was connected to a ventilator and then a dialysis machine for her failing kidneys. For a fortnight, Kali's medical team tirelessly worked to sustain her, navigating the delicate balance of preventing low blood pressure while halting episodes of high blood pressure exacerbating her brain swelling.
"We had good hours and bad hours, not days," recounted Dr. Linam. Gradually, Kali's brain swelling stabilized. Doctors reduced sedation and raised her body temperature, uncertain if she would be the same girl upon awakening. "We just didn’t know," admitted Dr. Linam, "but two days later, she did a thumbs-up, and her parents knew she was still in there."
Over the next eight weeks, Kali underwent the arduous process of relearning basic functions, including swallowing. Ultimately, she became the third officially documented survivor.
The precise reasons for her survival remain elusive. While a Florida boy of the same age, diagnosed shortly after Kali, did not survive despite receiving the same German medicine, Dr. Linam attributes Kali's recovery to a combination of divine grace and numerous fortuitous events—a series of small miracles that occurred daily, making the pivotal difference between life and death.
She Was “Dead” for 45 Minutes
They urgently rushed her back to the operating room.
Ruby Graupera-Cassimiro, a forty-year-old mother, had just undergone a routine C-section, welcoming a beautiful baby girl into the world on September 23. However, as her medical team transferred her to the recovery room, an unexpected event unfolded. Ruby, now a mother of two, slipped into a complete cardiac arrest.
Dr. Jordan Knurr, her anesthesiologist at Boca Raton Regional Hospital in Florida, swiftly intubated Ruby to facilitate mechanical breathing. He initiated a code, summoning around a dozen doctors and nurses into the room who vigorously provided advanced cardiac life support. "For over two hours, she experienced life-threatening heartbeats," recalled Dr. Knurr. The most concerning phase was when Ruby exhibited a pulseless rhythm—her heart beat, but it failed to pump blood throughout her body. Medical professionals tirelessly administered continuous CPR compressions for 45 minutes, aiming to restore her heart to normal function.
After a couple of hours, the medical team acknowledged the bleak outlook. They invited Ruby's extended family into the room to bid their farewells. Following their departure to the waiting room, accompanied by a few nurses fervently praying for a different outcome, the doctors ceased chest compressions. They were prepared to declare her time of death.
"I was on the verge of turning off the ventilation machine when one of the nurses yelled, 'Stop!'" recounted Dr. Knurr. "Without any medication or CPR, Ruby's heart spontaneously resumed beating after two hours. It's simply indescribable."
The cause was traced back to amniotic fluid leaking into the uterus, traveling through Ruby's bloodstream to her heart. Known as an amniotic fluid embolism, it induces an air block in the heart, hindering blood flow. Dr. Knurr admitted, "These embolisms are rare, and our understanding is limited. Typically, patients succumb to it or suffer significant brain damage." (The fate of the amniotic debris remains unknown; it is assumed to have dissolved naturally.)
Remarkably, Ruby not only survived but regained perfect health. Dr. Knurr marveled, "It's almost as if this never happened. It's a miracle. I'm not deeply religious, but occurrences like this are exceedingly rare." The following morning, Ruby's breathing tube was removed. Just four days later, she left the hospital with her newborn daughter, Taily, without even a fractured rib from the extensive chest compressions.
"Some higher force was in control that day; there's no doubt in my mind," asserted Ruby. "I don't comprehend why God chose me, but I'm certain he granted me this second chance at life for a purpose.
A self-repairing heart
He had been throwing up for four days. But clearly, this was not a mere stomach bug.
On August 17, 2012, 23-year-old Michael Crowe “froze up”—eyes open and staring into space—on the couch. He quickly snapped to, but when it happened again a few minutes later, his mother rushed him to the local emergency room.
There they learned that Michael was in real trouble. His heart was pumping out blood at just 25 percent, an alarmingly low rate. By the time he was transferred to Nebraska Medical Center in Omaha an hour later, it was down to 10 percent. A virus was causing acute myocarditis, inflammation of the heart muscle. If it got worse, he would need a heart transplant. With Michael’s family surrounding his bed, the doctors asked him to sign papers—while he still could—for that transplant. “They said I had only a 30 percent chance that my heart would recover,” Michael says. “I remember thinking, I can take those odds. I haven’t won the lottery yet, I’m Irish, I’m due for some luck. I was strangely calm.”
His doctors, however, were not. “His heart failure was so bad,” says his cardiologist, Eugenia Raichlin, MD. “The rate of mortality is huge.” They immediately hooked him up to an ECMO, an external heart and lung machine, to pump his blood while his heart couldn’t. But it was a short-term fix, and Michael’s health continued to decline. Spiking fevers led to convulsions; ice cooled him but dropped his oxygen levels. “It was a balancing game just to keep me stable,” Michael says.
For 17 days they waited, while Michael’s condition continued to worsen. His heart stopped twice—once for an entire day (being hooked up to the ECMO machine prevented him from dying). Doctors had to fend off blood clots and excess bleeding.
At 6:30 in the morning on Labor Day, Michael’s doctors got the phone call everyone had been waiting for: A heart would be available that night. But a few hours later, they made a devastating discovery. Michael had developed a blood infection; a transplant would be too dangerous.
As Michael’s family despaired, Dr. Raichlin noticed something unusual: His blood pressure, which should have remained constant because of the heart-lung machine, was actually rising. She ordered a test, which revealed that the left side of his heart was working at near-normal capacity. In disbelief, she ordered another. Again, the same astounding results.
After four days hooked up to a different machine that assisted only the right side of his heart, Michael no longer needed a transplant. His heart had completely, miraculously healed itself, his body eradicating the virus on its own. “He overcame everything,” Dr. Raichlin says. “He was very debilitated, but he rebuilt himself.”
Many patients with Michael’s condition die, get a heart transplant, or survive but have permanent heart tissue damage. But today, his heart is in perfect shape. “I’m so grateful that I got a second chance at life,” he says.




0 Comments